Featured Experts
Dr. Kaveh Alizadeh, a board-certified plastic surgeon in New York City
Dr. Gabriel Chiu, a board-certified plastic surgeon in Beverly Hills, CaliforniaJamie Gabel, PA-C and medical director at Advitam in New York City
Once a term known only by diabetics and pop culture aficionados, GLP-1 receptor agonist drugs are now part of the cultural zeitgeist. According to a recent poll, about 80% of Americans have at least heard of drugs like Ozempic—up 10% from last year—and one in eight of us has actually tried them. Ozempic and other medications like it are currently FDA approved only for the treatment of diabetes and obesity, but evidence shows they can also help treat issues like polycystic ovarian syndrome and even early Alzheimer’s (a Phase III clinical trial of semaglutide’s effects on the latter is underway). And, yes, it can work wonders for those who aren’t obese but just want to shed a few extra pounds.
Considering that a study out of University of California, Irvine estimated that nearly 93 million Americans are eligible for these medications on the criterion of obesity alone, we’re expecting that the patient population will continue to rise. But regardless of the reason for taking a GLP-1, users of these drugs know that there’s a learning curve. For example, you’ll quickly discover that eating too soon before bed can make for a rough night’s sleep.
Thinking about taking semaglutide or tirzepatide? Read on: with the help of experts, we’re sharing exactly what not to do when taking meds like Ozempic and Mounjaro, to make it easier to look and feel like your best self.
Don’t eat greasy, fatty foods
There are going to be several groups of foods and beverages that you’ll want to avoid while taking GLP-1 receptor agonists; chief among them, anything that’s high in fat. “Glucagon-like peptides work by affecting blood sugar and gastric emptying,” explains Dr. Kaveh Alizadeh, a board-certified plastic surgeon in New York City. The drugs stimulate insulin production and slow how quickly food moves through your stomach. Foods and drinks with high fat contents already move more slowly through your digestive system than others because it’s hard for your body to break them down. Think about how awful you can feel after a rich, heavy meal—on a drug like Ozempic, those crummy gastrointestinal side effects can last even longer. “These can include bloating, burping, nausea, diarrhea, and gas,” says Dr. Gabriel Chiu, a board-certified plastic surgeon in Beverly Hills, California.
Generally speaking, consuming high-fat foods puts strain on your body, which breaks down fats with bile, a substance produced by your liver and secreted by your gallbladder. “Fatty foods tend to cause more release of bile, which could potentially cause inflammation of the pancreas and the bile duct, thereby causing a potential gallstones or pancreatitis,” warns Dr. Alizadeh. This is a possible risk regardless of your GLP-1 status, but there’s evidence that these drugs can cause an increased risk of gallbladder disease, especially when used at high doses for long durations for weight-loss purposes.
Don’t eat big meals
Just as certain foods can stick around in your digestive system longer when you’re on a GLP-1 drug, so too can larger meals, which can leave you feeling uncomfortable at best and sick (to the point of vomiting, even) at worst. “In our experience, we advise patients to have less frequent meals and smaller portions, which also matches up with the drugs’ propensity to cause quicker satiety and feeling of being full after a meal,” says Dr. Alizadeh.
Don’t drink too much alcohol (if any)
If you’re someone who always craved a glass or two of wine at the end of a long day, you might find that Ozempic curbs your cravings—the drug’s manufacturer plans to study its effects on alcohol consumption and liver health due to evidence showing it can cause users to reduce their alcohol intake. That’s a good thing for a lot of reasons. Too much booze is bad for your health overall but especially while taking a GLP-1 receptor agonist. Beyond the fact that alcohol can have a lot of calories (and empty calories hinder weight loss), it can wreak havoc on your blood sugar. Your body stops producing glucose while you drink alcohol so that it can focus on metabolizing your cocktail. Meanwhile, one of Ozempic’s key functions is to lower blood sugar levels by helping your body produce insulin. As a result, “drinking alcohol while taking Ozempic may increase the risk of hypoglycemia,” says Dr. Chiu. “This can cause symptoms such as dizziness, confusion, lightheadedness, and shakiness.” (You’ll note those effects sound similar to those of being drunk!) While most diabetics will be aware of the risks of hypoglycemia, it may be new to those using the drug for weight loss.
According to Jamie Gabel, PA-C and medical director at Advitam in New York City, the combo of drinking alcohol and taking GLP-1 drugs can affect the pancreas. “GLP-1 peptides tell the pancreas to make insulin, an important process for getting sugar out of our blood and into our muscles, brain, and wherever else it is needed,” he explains. “Alcohol can irritate the pancreas, so both of them together can further irritate the pancreas and possibly cause pancreatitis.” It’s worth noting that pancreatitis (as well as hypoglycemia) are possible side effects listed on Ozempic’s warning label.
If you’re struggling to curb your drinking, whether you’re on a GLP-1 medication or not, and want to quit for your health and weight-loss goals, our editors have found Going Dry: A Workbook: A Practical Guide to Drinking Less and Living More by Hilary Sheinbaum to be a helpful tool for assessing their relationship with alcohol, setting benchmarks, and tracking their progress along the way.
Don’t inject the medication too frequently
While there is a pill form of semaglutide (Rybelsus), all other GLP-1s on the market are injectable. Liraglutide (Saxenda and Victoza), the earliest GLP-1 drug to receive FDA approval, is meant to be injected daily, but semaglutide (Ozempic and Wegovy) and tirzepatide (Mounjaro and Zepbound) are supposed to be administered weekly. How often you inject these drugs has to do with their half-lives and how long they stay in your system. “Each drug has what’s called a half-life, which means the time that it takes to reach half of its effective dose in the bloodstream,” explains Dr. Alizadeh. “The way we decide how long or often to take a drug is based on the half-life.”
For context, liraglutide has a half-life of 13 hours, meaning that in about three days, it’ll be fully excreted, so you need to inject it daily to keep the levels steady in your body. “Semaglutide can stay in your system for up to five weeks and has a half-life of seven days,” says Dr. Chiu. As a result, you should inject it every week, though he shares that some people can stretch it to 10 days without losing efficacy or experiencing adverse effects. “Injecting more often [than every seven days] could give you symptoms similar to overdosing—hypoglycemia, nausea, stomach pain, vomiting, and increased risk of pancreatitis,” he warns.
Don’t eat right before bedtime
According to the Sleep Foundation, eating anywhere from two to four hours before bed is best, though one study that shows a small presleep snack can help build muscle (more on this shortly). “Our cells and bodies go to work on many functions when we go to sleep,” says Gabel. But breaking down your food isn’t one of them, which is why most people don’t feel great going to bed immediately after eating, regardless of whether they’re taking semaglutide. “We sense this as feeling bloated and distended, acid reflux, and indigestion.” With the delayed gastric emptying of GLP-1s, the severity of those symptoms increases. Adds Dr. Alizadeh, “it can lead to constipation and severe abdominal pain that may even necessitate going to the emergency room.”
Don’t forget to drink plenty of water
There is some evidence that drinking more water can help support weight loss, but that’s not why it’s important to get enough H2O when on GLP-1s. According to Dr. Chiu, dehydration is an issue when you are on Ozempic or Mounjaro, so reduced water intake could cause bigger issues, including kidney problems and urinary tract infections and serious constipation. Drinking plenty of water will help your body flush waste out of your system.
Without enough water, you . also pass out. Lightheadedness and fainting can occur when anyone is dehydrated, but the risk is heightened on GLP-1 drugs. “These medications are hormonelike substances that can affect the regulation of your blood sugar and your blood pressure,” explains Dr. Alizadeh. “Dehydration can quickly cause a short-term change in your heart rate and blood pressure—on a hot summer day, you have an additional risk of your vessels dilating in response to heat, which can then potentially cause a circulatory collapse.” To boost your body’s hydration levels, consider drinking beverages with added electrolytes.
Don’t get on the medication without talking to your doctor
Semaglutide and other GLP-1s are touted as miracle drugs, but that doesn’t mean they’re for everyone. “Used improperly or without knowledgeable supervision, semaglutide can cause serious harm,” warns Gabel. Adds Dr. Alizadeh, “It’s extremely important for you to have a qualified healthcare provider managing these medications, because they are affecting multiple systems within your body—and if they’re not managed correctly, it can have devastating consequences, such as nausea, vomiting, and constipation on the one end and hospitalization and surgery on the other.”
Anecdotally, we’ve seen many of our friends and family members have great success with GLP-1 medications, but we’ve also seen a handful of people experience some pretty bad side effects—and in several instances, those individuals got semaglutide or tirzepatide off the internet, including via telehealth programs. “If you are serious about getting results, you need to have blood work performed before starting the medication, to have a baseline of your lab values, and a complete physical, to make sure you are a good candidate,” says Dr. Chiu, who does not recommend starting the GLP-1 journey online. “The problem with the telehealth programs is that if there is a problem, your only outlet is to go to the emergency room,” says Dr. Alizadeh.
Seeing a provider in person will provide you with ongoing supervision and support, which will help ensure that you’re responding properly to the medication and manage side effects. “It is an incredible medication with amazing benefits, but you need to be properly monitored to ensure safety and optimal efficacy,” confirms Gabel. While you can have success with telehealth companies, you’ll need to do your homework to find a good one—the provider should be very thorough and discuss your medical history with you (including that blood work), send you for a body composition analysis, and set up follow-up appointments instead of just giving you automatic refills, says Gabel. “Cheaper isn’t always better—you get what you pay for,” he says.
Don’t rely on GLP-1s to “keep you healthy”
Losing weight without working out or subsisting exclusively on salads sounds like a dream to many, and yes, these drugs can deliver—but that’s really not the right approach to taking a GLP-1. “It’s not just about taking this medication to hit your goal. You also have to incorporate a lifestyle change, which at the minimum, requires you to engage with physical activity to help your body build up as you lose the calories from these medications,” says Dr. Alizadeh.
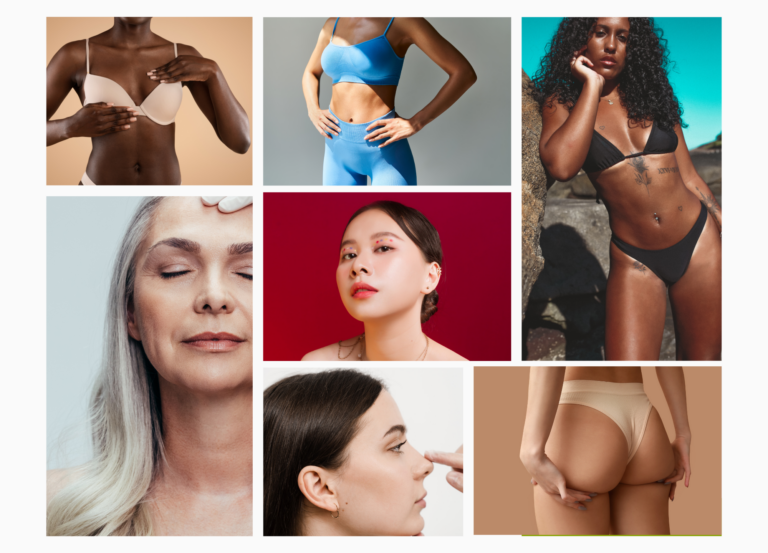
According to Gabel, GLP-1s cause muscle cells to dehydrate. Muscles burn more calories than fat, and dehydration can lead to muscle loss; the combo of the two is what can cause the dreaded “Ozempic face” or “Ozempic butt.” All of our experts recommend pairing GLP-1 use with resistance training to maintain muscle mass and tone as you lose weight. “Focusing on a high-protein diet is also very important to prevent muscle loss,” adds Dr. Chiu.
Don’t let aesthetic concerns prevent you from trying the medication
A lot of people take semaglutide because they want to “look better,” but we can understand how a saggy face and butt don’t sync up with that goal. First of all, know that it’s not the weight loss caused by Ozempic but the speed at which you accomplish it that can cause “Ozempic face.” We understand the appeal of near-instant gratification, but slow and steady truly does win the race. “Relatively quick, drastic weight loss is more likely going to result in loss of muscle tone and mass, poor recovery of skin elasticity, and tissue laxity,” explains Dr. Chiu. “Slowly increasing your dosage allows your tissues to respond to the weight loss appropriately.”
However, it’s often much easier to fix sagging skin than the many health concerns caused by carrying around excess weight. “For patients who are overweight or obese, the most important objective is to get them close to their ideal body weight, because we’re then able to treat their high blood pressure, obstructive sleep apnea, joint problems, and heart problems,” says Dr. Alizadeh. “Once we are able to get you to an ideal body weight, Ozempic face, Ozempic butt, or excess skin are very easy problems for a highly trained specialized plastic surgeon to fix.”