If you’ve ever had major plastic surgery before (the kind that involves general anesthesia and significant downtime), you know that recovery can be brutal. Physical pain aside, it’s quite common to feel lightheaded and dizzy, dehydrated, exhausted, and just plain worried about the blood loss or oozing that you’re seeing post-procedure. It’s for this reason that some plastic surgeons—predominantly those in Miami, America’s plastic surgery hot spot—have started to integrate a special form of technology into their operations: cell savers.
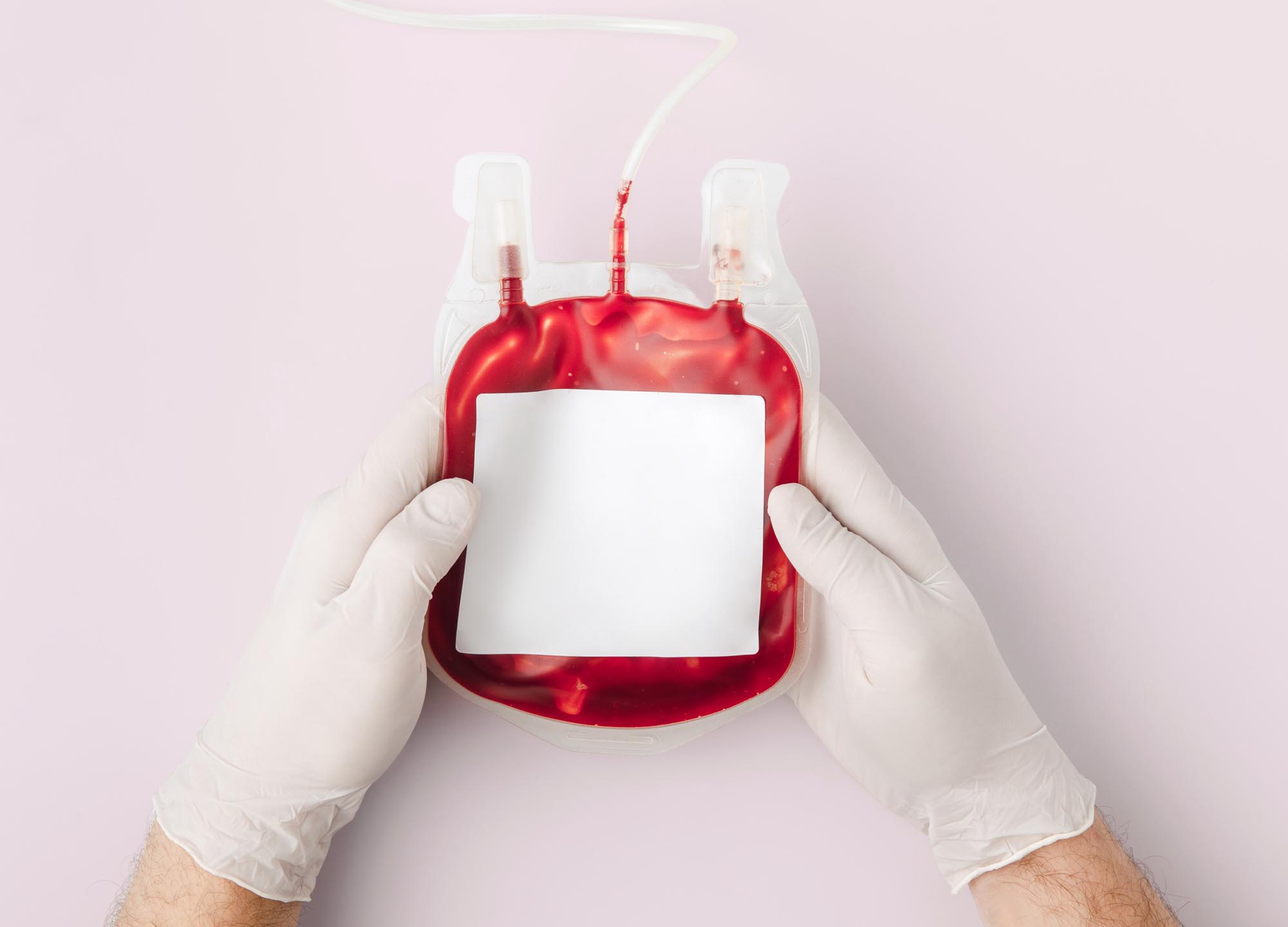
“The cell saver device is a machine that captures the blood from the surgical field in a sterile manner,” explains Dr. Moises Salama, a board-certified plastic surgeon in Hollywood, Florida. That blood is taken into the machine via surgical cannula. From there, the blood is centrifuged, separating the red blood cells from all other impurities, such as IV medicine and fat.
“You know, from Grandma’s gravy, that if you put it in the fridge, the fat goes to the top and then you’re going to get a lot of fluid in at the bottom,” explains Dr. Jonathan Fisher, a board-certified plastic surgeon in Miami. (The centrifuged fat is either disposed of or reserved and processed for fat transfer, if desired.) Once the blood has been filtered and cleansed of all remaining fat cells, antibiotics, or anything else, the healthy blood cells that remain are “transfused back to the patient sterilely, in a closed system,” explains Dr. Salama. This acts as something of a self-transfusion. The whole cell saver blood-cleansing process takes 20 minutes or less and is usually performed during surgery “halftime,” says Dr. Fisher, when a doctor flips a patient over halfway through the procedure to work on the other side of their body.
If cell saver technology is a new concept to you, you’re not alone. Traditionally, the use of cell savers was reserved for procedures that could result in significant blood loss, such as orthopedic surgery, open heart surgery, and other riskier procedures, typically in a hospital setting, notes Dr. Salama. However, in recent years—in large part, due to the doctors in this article and other intrepid Miami-area plastic surgeons—cell savers have hit the plastic surgery scene, where they’re typically used during liposuction and fat transfer, though they can be used “during any surgical procedure in which blood loss can affect a patient’s well-being,” adds Dr. Salama. And while liposuction is typically very safe and blood transfusion is uncommonly needed during that operation, the discomfort post-procedure can be significant.
According to Dr. Fisher, before using the cell saver, his patients would often skip their follow-up appointments because they felt woozy and uncomfortable. “More importantly they weren’t eating, they weren’t drinking, and they weren’t getting out of bed, because they felt so bad that all they wanted to do was lie around.” This is problematic for two reasons: Getting up and walking around the day of surgery is extremely beneficial to the healing process, and uncomfortable patients tend to go to the hospital emergency room (even after being reassured that they’re perfectly fine and experiencing normal pain), where a provider may end up giving them an unnecessary and potentially risky blood transfusion.
“Cell saver transfusion does not carry the same risks as conventional pressure-regulated volume-control transfusion because patients are receiving their own blood as opposed to someone else’s blood,” says Dr. Salama. (Unfortunately, your provider won’t be able to bank that blood for future use unless they have a blood bank license.) While there are risks to cell saver transfusion—such as infection and receiving hemolyzed blood (broken blood cells)—it’s very, very uncommon. “To my knowledge, with all the people I know in town, thousands and thousands of cell saver procedures have been performed, and I haven’t heard of any complications at all—zero,” adds Dr. Fisher.
If you’re curious to know if you’re a candidate for cell saver, both doctors in this article would likely say yes, even without having met you. “Any patient receiving their own blood, retransfused via cell saver, will benefit more than those who receive plain IV fluid therapy,” says Dr. Salama. Dr. Fisher mandates the use of cell saver for some patients, including those with a higher BMI, patients over 40, and patients with a hemoglobin level below 12.5 (normal is 13.5–17.5 for men, 12-–5.5 for women).
Dr. Fisher also requires that all his male patients use cell savers. “Men are horrible patients—they’re weak,” he says. “They’re not used to getting plucked and waxed, they don’t have periods every month… if their hemoglobin goes down to 15, they think they’re dying.” But truth be told, even patients who don’t meet his requirements often integrate a cell saver into their procedure. “This has almost completely eliminated people going to the emergency room or even thinking about it,” Dr. Fisher enthuses. As a self-described “big believer” in cell saver technology, he will soon be traveling to France to lecture about it and perform live surgery using it. “They have it in Europe, but nobody’s using it for [plastic surgery],” he says.
While many providers who use cell saver technology incorporate it into the overall cost, others charge a bit more for the service. “Cell saver is an add-on to our surgical procedure packages because it is based on recommendation for the patient,” says Dr. Salama, who charges an additional $500 for the use of cell saver during his operations. But even if a provider eats the cost, using a cell saver simplifies both their and their patients’ lives. “In my opinion, it is very beneficial to patients,” Dr. Salama adds. And considering that it’s a small price to pay for added peace of mind and enhanced post-procedure comfort, we’d have to agree.