Ah, Ozempic—quite possibly the most talked-about and polarizing FDA-approved injection since Botox. In case you’ve been offline the past six months, Ozempic and Wegovy are brand names for semaglutide, a glucagon-like peptide (GLP-1 antagonist) that is essentially a string of amino acids that, once injected, decreases blood sugar level and suppresses appetite. Initially used to treat diabetes, Ozempic was first approved for medical use in patients with type 2 diabetes, to regulate blood sugar levels, manage weight, and decrease the risk of cardiovascular disease. However, in June 2021, the U.S. Food and Drug Administration approved Wegovy for long-term weight management and triggered a whirlwind of hot takes on who “should” and “shouldn’t” be using the drug. (The Real Housewives even joined the conversation.)
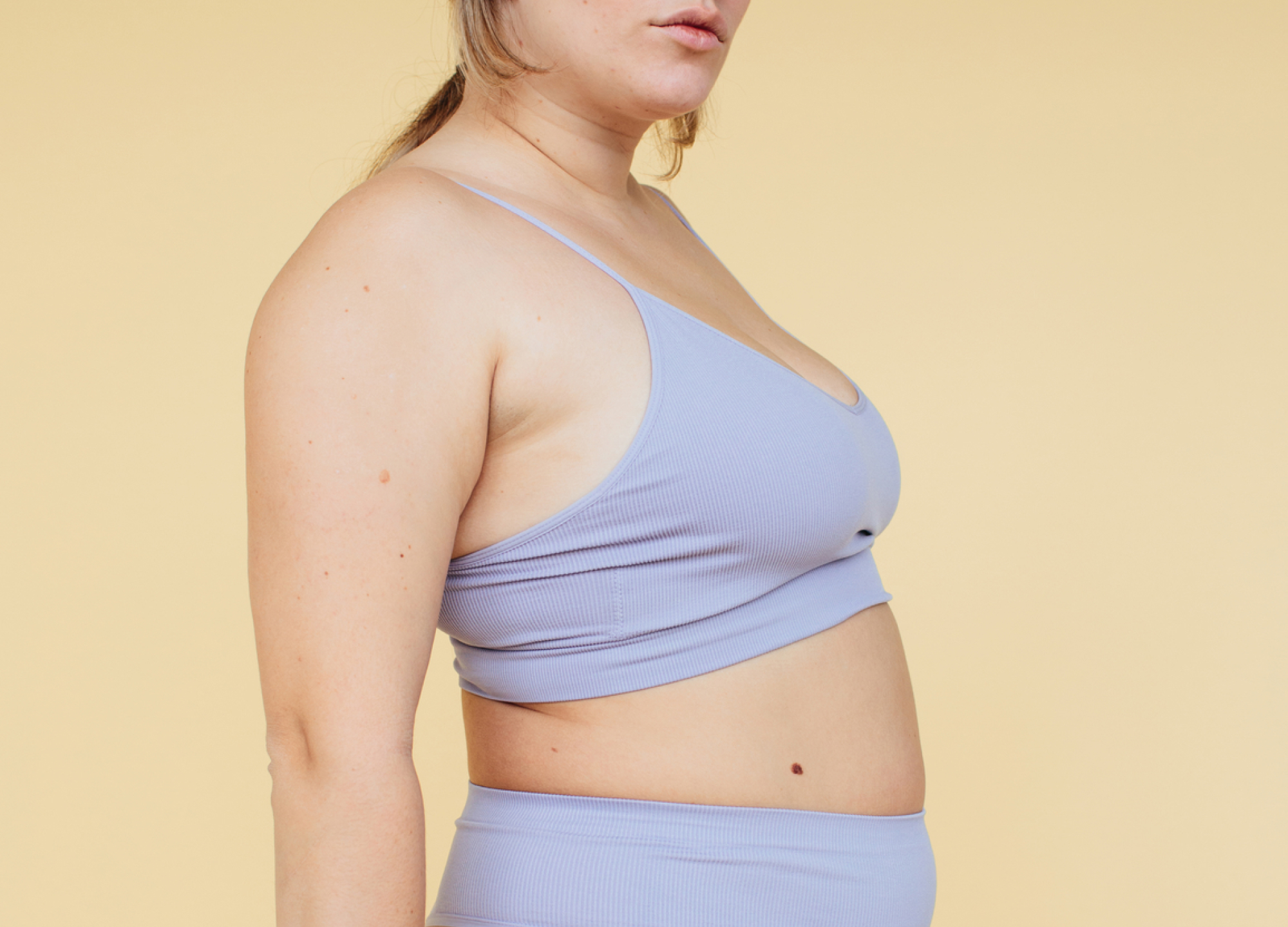
For people like me, who’ve been overweight and dealt with weight fluctuations their whole life, taking semaglutide for weight loss sounds like a dream. Why? Because losing weight “naturally”—i.e., without surgery or prescription medication—is very hard. Trust me, I’ve done it. From May 2017 to May 2018, I lost 100 pounds through diet and exercise alone. No procedures, nutritionist, personal trainer, or health coach—just protein shakes, detoxifying cleanses, a bit of intermittent fasting, and my Planet Fitness membership. But let it be known: it wasn’t just casual dieting and exercise. This kind of weight loss was “achieved” by eating 1,000 calories or less and exercising up to four hours a day. (Like I mentioned, I was not under a physician’s guidance at this time and would not recommend following this plan.)
I was a newly freelance writer in New York City, with a flexible schedule that allowed me to commit to this intense lifestyle and a budget that forced me to say yes to walking everywhere and barely spending money on food. I weighed 250 pounds on May 1, 2017, and 150 pounds by the end of April 2018.

Due to how unsustainable my weight-loss journey was, maintaining my new weight proved to be a challenge. Somewhere between the middle and end of 2019, I began upping my calories and decreasing the hours spent moving my body on a daily basis. Then came the pandemic. Like most people who did not have a front-line job, I spent the majority of 2020 indoors, sitting in front of a screen, doing little exercise. As a result, since 2019 I’ve regained about 70 pounds and that weight hasn’t easily come off with more casual exercise and intuitive eating.
When the chatter began that celebrities were using Ozempic as a way to shed weight and get red carpet ready quickly, I felt defeated at first. I was finally at a place where I was accepting of my regain after such drastic weight loss, and then came society telling me that the body-empowerment movement is over and we’re idolizing smaller bodies again. But then I realized I was a candidate for this drug and could use it to feel more comfortable—physically and mentally.
For my prescription, I sought out Dr. Azza Halim, a board-certified anesthesiologist and regenerative medicine physician with offices in Florida, California, and Illinois, who says that candidates for semaglutide are prediabetics, those with a BMI greater than 30, or those with BMI of 27 who also have other underlying health issues such as high blood pressure, high cholesterol, or metabolic syndrome/diabetes. When it comes to drug interactions, Dr. Halim advises against combining Semaglutide with any type of insulin, acetazolamide, anticonvulsants, tricyclic antidepressants (such as amitriptyline, nortriptyline), or monoamine oxidase inhibitors (MAOI).
For patients who are not prediabetic and have to pay out of pocket, the price of prescription semaglutide depends on the brand, your doctor, and where you’re located but can be an average of $1,750 a month. In comparison to the little money I was spending on my weight-loss journey a few years ago, semaglutide is obviously more costly.
Weight loss with Ozempic
For the first four weeks, Dr. Halim prescribed me 0.25 mg of semaglutide and I lost about eight pounds. For the second month, Dr. Halim increased my dosage to 0.5 mg and I lost an additional four. So in two months on semaglutide, I’ve lost 12 pounds. This is similar to the rate at which I lost weight the first time around. However, in the past eight weeks, I have not been as mindful of calories and have not worked out as often as I did before. Dr. Halim told me that, according to the semaglutide clinical trials, “the average weight loss is 6% of [your body] weight by week 12 and 12% by week 28.” She recommends staying on the drug for at least 12 weeks in order to let the body adapt and to see changes.
As for side effects, you’ve likely heard horror stories about the nausea and discomfort users have experienced. I had a bit of nausea the day after gettingmy first dose and once more after I felt like I’d overeaten, but the nausea hasn’t been consistent or unbearable by any means. And whether you consider a suppressed appetite a side effect or something to celebrate, that is my biggest takeaway from the drug. I simply do not feel hungry, so my brain does not let me think about eating nearly as often as I used to. Throughout my first weight loss, mentally fighting the urge to habitually overeat and make unhealthy choices was by far the hardest part. With semaglutide, that urge is simply not there.
As eager as I was to start my semaglutide journey, I was equally terrified to put my entire weight-loss journey down on digital paper. Openly admitting that I once lost 100 pounds naturally, then gained a lot of it back and am now resorting to what many in society deem a “shortcut” or “cheat” feels like I failed—even though I know I didn’t. The truth is, losing weight naturally is extremely difficult, and taking semaglutide makes it easier. I shouldn’t have to struggle just to feel good in my body.